Megasphaera type 1 is a prominent type of bacteria linked to bacterial vaginosis (BV), a common vaginal infection.
This blog post will discuss Megasphaera type 1, its relationship with bacterial vaginosis, and the various treatments and preventive measures available for those affected by BV.
Key topics in this post include:
- What is Megasphaera type 1 and its role in bacterial vaginosis
- Symptoms and diagnosis of BV
- Treatment options and medications
- Preventing bacterial vaginosis from recurring
What is Megasphaera Type 1 and Its Role in Bacterial Vaginosis
Megasphaera type 1 is a species of anaerobic bacteria that can be found in the human vagina.
Although not inherently harmful on its own, an overgrowth of Megasphaera type 1 can lead to bacterial vaginosis.
BV occurs when there is an imbalance of good and bad bacteria in the vaginal area, often resulting from the overgrowth of bacteria, such as Megasphaera type 1 and others like Gardnerella vaginalis.
This imbalance can disrupt the natural ecosystem of the vagina and lead to a variety of symptoms and complications, making it important to address BV effectively.
Symptoms and Diagnosis of BV
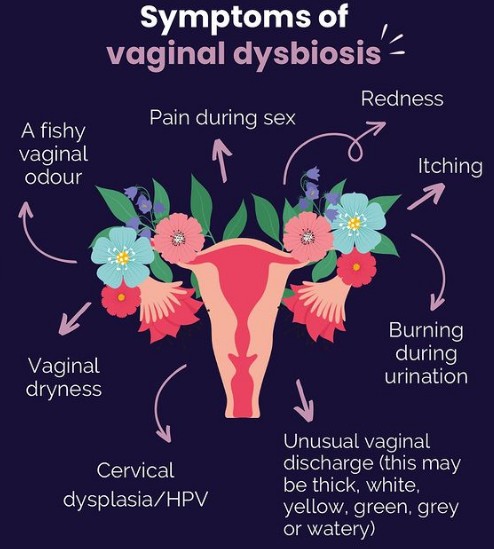
Bacterial vaginosis can present with several symptoms. Some common BV symptoms include:
- Thin, grayish-white discharge
- Fishy odor, especially after sexual intercourse
- Itching or burning in the vaginal area
- Pain or discomfort during sex or urination
Many of these symptoms resemble those of other vaginal infections, such as yeast infections, which makes getting an accurate diagnosis from a healthcare professional crucial.
To diagnose BV, a healthcare provider will typically perform a physical examination, review the patient’s medical history, and take a sample of vaginal discharge for lab testing.
This thorough evaluation ensures appropriate treatment can be administered to provide relief and prevent complications.
Treatment Options and Medications
Several medications are available for treating bacterial vaginosis.
The most common are antibiotics, which can be prescribed in oral or topical forms.
Oral antibiotics, such as metronidazole or clindamycin, are generally taken for 7 days, while topical treatments, like clindamycin cream or metronidazole gel, are applied directly to the vagina.
In some cases, over-the-counter (OTC) medications and natural home remedies may provide relief for mild BV symptoms.
However, always consult a healthcare professional prior to trying any alternative treatments to ensure safe and effective care.
Preventing Bacterial Vaginosis from Recurring
Bacterial vaginosis can recur in some individuals, even after successful treatment. Adopting preventative measures can help reduce the likelihood of recurrence:
- Probiotics: Supplementing with probiotics, such as Lactobacillus, can help maintain a healthy balance of good bacteria and support overall vaginal health.
- Maintain proper vaginal hygiene: Avoid using harsh soaps, douching, or scented products, as these can disrupt the natural pH balance of the vagina.
- Practice safe sex: Using condoms consistently and limiting sexual partners can reduce the risk of contracting BV and other sexually transmitted infections.
Conclusion
Megasphaera type 1 is a bacterium involved in the development of bacterial vaginosis.
Understanding its role, recognizing BV symptoms, and seeking professional healthcare advice for diagnosis and treatment are crucial to effectively manage this condition.
With proper care, bacterial vaginosis can be successfully treated, and adopting preventive measures can minimize the chances of recurrence.
